
Measuring “Experience” in Value-Based Specialty Care (Part 2 of 3 of Applying Porter’s Framework for Health Insurance Plans)
Protera’s Points:
· The purpose of this series is to help health plans implement a framework for assessing “value” of specialty care provided to its members.
· This assessment will improve health outcomes, costs, and experience for members
· It will also allow facilitate prioritization (in steerage and/or reimbursement) of high-value providers
· When considering Porter’s framework for measuring value, the numerator (outcomes) consists of two parts: clinical outcomes that matter to the patient as well as patient experience. The denominator is cost of care provided.
· Health plans must be able to quantitatively assign value scores to their specialty providers in order to optimize outcomes and costs for its members and partners’ (i.e., self-insured employers) members
· Part 1 of this series provided an overview of clinical outcomes (PROMs); Part 2 will review experience measures and how to combine both components into a quantitative “numerator”
· We are taking the abstract (“value equation”) and turning it into an actionable playbook for health plans.
Introduction
In Part 1 of this series, we introduced the healthcare value equation, as proposed by Professor Michael Porter from Harvard Business School. We also dove into the numerator of the equation, focusing on outcomes that matter to the patient and how to incentivize providers for collecting and reporting them to the plan (to access Part 1, please click here for the LinkedIn version or here for the web version).
In Part 2, we will focus on the second half of the numerator: experience (referred to as “service” in the formula below). Together, with outcomes that matter to patient, we get the full numerator (“outcomes”) of the value equation.

There are many ways to measure patient experience, and there is certainly no shortage of surveys and assessments that patients are bombarded with every time they go to a medical facility. Moreover, health plans are already collecting a number of experience measures (STARS, CAHPS, HOS, Star Ratings). So why do we need to collect more data?
Because of the financial incentives associated with costly procedures and surgeries, health plans (along with their risk-bearing partners and employers) must ensure that this costly specialty care is of high value (improved health outcomes and/or lower costs of care, ideally both!). To ensure this, health plans must be able to measure value of specialty care episodes, as opposed to global satisfaction. Successful measurement will allow health plans to prioritize high-value providers (through steerage and/or enhanced fee schedule) and de-prioritize low-value providers.
Currently, provider value assessment is largely relegated to costs of care. Most would argue that the quality of care – outcomes and experience – must be considered in addition to costs. We have already discussed half of the outcomes component (PROMs); now, let’s dive into experience measurement.
Patient Experience – a Framework
Rationale
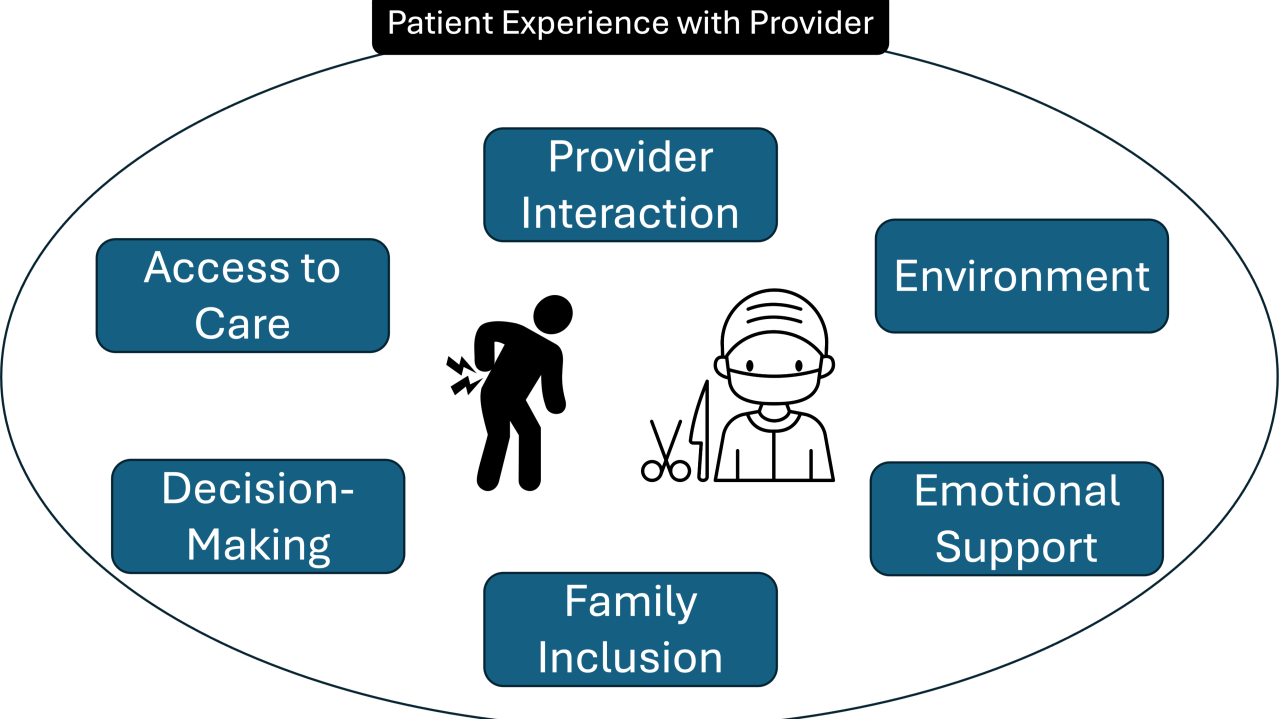
Patient experience encompasses many components. These include access to care, communication, coordination of care, provider interaction, environment, emotional support, and inclusion of family members/care givers. These factors can be uniquely measured with respect to health plan, healthcare facility, and healthcare provider. Patients can have very different assessments of these three groups with regards to experience ratings. Therefore, health plans must measure patient experience as it relates to the specialty care provider.

Resistance to this might include the argument that health plans are already measuring numerous experience measures. For example, Medicare Advantage plans expend significant energy in their Star Ratings. Core components of Star Ratings include preventative care (i.e., screening tests and vaccine compliance), chronic disease management, global ratings of care access/quality, member complaints, and customer service.
If a health plan is trying to optimize value of total joint replacement, the above factors give little direct indication of the experience ratings of the providers that are performing joint replacement surgery. To successfully measure experience, health plans must do the following:
1 – identify questions/assessments for a given condition or episode
2 – collect responses from members within that condition or episode at defined time-points
3 – normalize responses into a reference scale which can be used to compare providers
Step 1 – Identify questionnaires for collection
First, health plans must identify what experience components are most important for measurement. Our recommendation is to focus on 2-3 core components, such as provider communication, participation in shared decision-making, and willingness to recommend that provider to family or friends. These domains can help assess the patient’s perception of trust and confidence in their specialty provider.
Once these priority components are determined, question prompts must be identified. There are numerous validated patient reported experience measures (PREMs) currently used, but these can be quite lengthy. It may be instead beneficial to identify a subset of questions (being mindful of any relevant copyright considerations) that align with the high-priority core components. In formulating these assessments (ideally no more than 5 questions), health plans can partner with third-party companies such as Press Ganey or can create their own custom questionnaire. We recommend incorporating a “Likert Scale” for the responses to aid in quantifying the data.
Step 2 – Collect responses from members
Unlike PROMs, experience measures do not need to be collected both before and after an intervention. Instead, they can simply be collected at a practical and defined time within or after the episode (i.e., 6 months after total joint replacement, 90 days after prostate removal, etc.). Lags in claims processing may require a questionnaire assignment slightly later in the episode than otherwise would be selected.
To implement assessment collection, health plans have three options: outsource to third party company, rely on providers to report, or collect themselves. Either option is reasonable. It is important to note that any post-intervention collection of data requires some element of human effort, as passive electronic collection is inadequate for proper sampling (as reported in several clinical studies from our team[1],[2]. While it is easiest to rely on providers to submit experience data, it is challenging (if not impossible) to standardize the questions of the assessment.
Step 3 – Normalize responses
Once the health plan has identified target questions and implemented a collection plan, it must score this data to facilitate comparison of providers. As mentioned, using a Likert Scale response system is an easy approach, as each question can be scored on a scale of 1-5.
For example, a four-question experience assessment, each with a 5-item Likert response (example below), can easily be turned into a quantitative score. In this example, the total score would range between 4 points (lowest possible score) to 20 points (highest possible score).

Looking ahead to Part 3: Measuring Costs
Next week, we will round out the three-part series with an article about cost measurement for value-based specialty care assessments.
Ready to get started with value-based specialty care?
If you are a ready to implement value-based specialty care transformation (including the topics from this newsletter) in your healthcare organization, we may be able to help. Our expert team at Protera Health has over a decade of experience in implementing these initiatives at health plans and delivery organizations.
We help health plans and risk-bearing organizations improve outcomes and lower costs for musculoskeletal (MSK) conditions. We do this through a virtual-first, multidisciplinary approach with services delivered through in-network contracting (no administrative budgeting needed!).
To get started, book a demo with us or learn more at our website.








